Press Release
Contact
Molly McDougall
HealthFlash Marketing
203-431-4000
molly@healthflashmarketing.com
Sharon Grutman
The American Society of Breast Surgeons
877-992-5470
sgrutman@breastsurgeons.org
Download
Download PDF
Download Word
Slides - coming soon
Well-Selected Nipple-Sparing Mastectomy Patients with Elevated Risk Experience Low Rate of Complications
- Abstract: Outcomes of >1300 Nipple-Sparing Mastectomies with Immediate Reconstruction: The Impact of Expanding Indications on Complications
Dallas, May 2, 2019--Nipple-sparing mastectomy complication and implant failure rates have decreased significantly since introduction of the procedure, while the patient population increasingly includes more advanced cancers and women traditionally considered at risk for post-surgical difficulties, according to a new study presented this week at the annual meeting of the American Society of Breast Surgeons. Researchers examined surgeries performed on 1301 breasts in 769 women who retained their own nipples and skin for breast reconstruction following mastectomy from 2009 to 2017 at a major institution.
“Research continues to validate the oncologic safety and enhanced cosmesis of nipple-sparing mastectomies,” comments lead researcher Tina Hieken, MD of Mayo Clinic. “Our perception has been that these procedures are increasingly performed on far more complex cases from an oncologic and technical standpoint. However, the results of this study were striking. It not only confirmed this but showed that these surgeries can safely be offered to a far more diverse and challenging group of well-selected patients.” Nipple-sparing mastectomy was performed occasionally starting in about 2001 and has steadily grown in use.
The study retrospectively examined the 30-day rate of complications that required treatment and one-year reconstruction failures from a prospective Mayo Clinic surgery database. Complications ranged from surgical site infections, hematomas and seromas requiring surgery to necrosis requiring tissue removal as well as unplanned additional surgeries. Among the patient and tumor variables examined were obesity (>30 BMI), recent or current smoking, neoadjuvant chemotherapy, node-positive breast cancer/prior breast surgery and prior radiation.
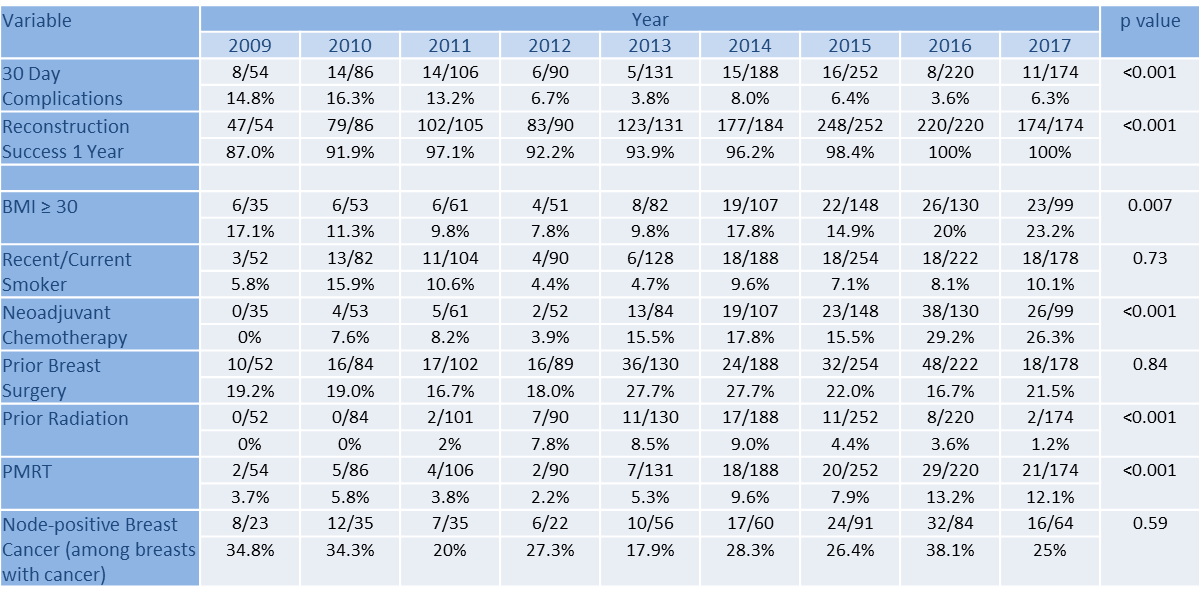
The overall nipple-sparing surgery complication rate declined from 14.8% in 2009 to 6.3% in 2017 with an average rate of 7.5% for this eight-year period. One-year reconstruction success rose from 87% in 2009 to 100% in 2017. During this time, the number of patients classified as obese, an acknowledged risk factor for complications from these surgeries, rose from 17.1% in 2009 to 23.3% in 2017. No patients receiving neoadjuvant chemotherapy were treated using the procedure in 2009, while they made up 26.2% of the population in 2017, suggesting inclusion of higher risk cancer patients in the surgical current pool.
Surprisingly to researchers, after 2013, obesity was no longer associated with any negative outcomes, while risk factors of prior radiation and smoking significantly increased complications. Prior radiation also was heavily associated with one-year reconstruction failure.
“Nipple-sparing mastectomies are difficult procedures, requiring highly perfected skillsets and engagement from the entire surgical team,” comments Dr. Hieken. “Breast surgeons, reconstructive plastic surgeons, oncologists and skilled nurses must be committed and practiced at working seamlessly as a group to make these surgeries a success. Over the years, techniques, teamwork and patient selection at Mayo Clinic, and likely at other hospitals, have been optimized to enhance results.”
For example, Dr. Hieken notes that surgeons have learned that incision placement, such as avoiding the areola, can be optimized for better cosmesis and fewer complications. Technology such as SPY angiography, a specialized intraoperative procedure, helps to assess the perfusion and viability of flap tissue. Bundled interventions specifically focused on minimizing infections have also made a difference.
“Offering enhanced aesthetics as a result of surgeries like this to women who have had a devastating diagnosis is extremely rewarding,” she says. “Today, breast cancer patients who are not offered nipple-sparing procedures should ask their surgeons why. As this study demonstrates, these surgeries are proving safer for a far broader patient base.”
Expert Commentary:
The investigators at Mayo Clinic achieved excellent results in improving 30-day and one year reconstruction rates in patients undergoing nipple-sparing mastectomy. They clearly demonstrated that careful patient selection and a multi-disciplinary team can improve outcomes over time. This data can educate other surgeons on important factors for patient selection as well as techniques to improve outcomes. We look forward to the long-term oncologic safety data in this higher risk cohort.
Sarah Blair, MD, FACS
University of California San Diego, ASBrS Publications Committee Co-Chair
Abstract, Official Proceedings
Outcomes of >1300 Nipple-Sparing Mastectomies with Immediate Reconstruction: The Impact of Expanding Indications on Complications
Authors: Whitney Young, Amy Degnim, Tanya Hoskin, James Jakub, Minh-Doan Nguyen, Nho Tran, Christin Harless, Oscar Manrique, Judy Boughey, Tina Hieken
Institutions: Mayo Clinic, Rochester, MN
Background/Objective: The enhanced aesthetics and demonstrated oncologic safety of nipple-sparing mastectomy (NSM) in well-selected patients has resulted in increased rates among patients with locally advanced breast cancer and those with risk factors such as obesity and prior radiation and surgery. Limited data exist on the complication and reconstruction success rates in a contemporary patient cohort with expanded indications for NSM. Thus, our aim was to evaluate these metrics over time as indications for NSM and patient selection criteria have evolved.
Methods: With IRB approval, patients treated with NSM from 2009 to 2017 were identified from our prospective breast surgery registry. Main outcomes were 30-day complication requiring treatment (surgical site infection, hematoma or seroma requiring operation, necrosis requiring debridement or hyperbaric therapy, unplanned reoperation) and one-year reconstruction failure rates. Patient, tumor and treatment variables of interest were analyzed. Cochran-Armitage trend tests were used to evaluate significance of changes over time; risk factors for complications and reconstruction failure were assessed using logistic regression.
Results: We evaluated 1301 breasts in 769 women undergoing cancer treatment (n=542) or risk reduction (n=759). Median patient age was 48 years (range: 21-77). The overall 30-day complication rate was 7.5% (97/1301 breasts) and declined from 14.8% in 2009 to 6.3% in 2017, p<0.001, despite a significant increase over the study period in the proportion of patients with obesity (p<0.001) and treatment with neoadjuvant chemotherapy (p<0.001) as shown in the table. Reconstruction success at 1 year was 98.5% among 1281 evaluable breasts. Obesity was not significantly associated with either outcome after 2013. Prior radiation (OR 2.3, p=0.04) and recent/current smoking (OR 3.3, p<0.001) significantly increased the risk of 30-day complications. Prior radiation was significantly associated with reconstruction failure at one year (OR 4.6, p<0.001) as well as adjuvant radiation therapy (OR 3.3, p=0.002).
Conclusions: We found decreasing 30-day complication rates of NSM, despite broadened indications among higher-risk patients over time. These data confirm a team learning curve with NSM and also demonstrate the nipple-sparing approach is suitable for appropriately selected higher-risk patients for both risk reduction and cancer treatment.